Hypoglycemia
Hypoglycemia is a major limiting factor in the glycemic management of type 1 and type 2 diabetes. In patients with type 2 diabetes, severe hypoglycemia has been shown to be the most common acute adverse effect of glucose-lowering therapy and it is associated with poor outcomes.1 Mortality rates associated with key trials have demonstrated that severe hypoglycemia is significantly more likely in patients who received intensive glycemic control, presenting a challenge for clinicians who seek both to control blood glucose levels and to provide better patient outcomes. Patients who experience hypoglycemia typically have a long duration of diabetes, a known history of hypoglycemia, advanced atherosclerosis, and/or advanced age/frailty. Therapeutic blood glucose targets should be personalized and evidence suggests that patients who experience hypoglycemia may benefit from less aggressive glycemic control. The selection of pharmacologic therapies should take into account a patient’s cardiovascular risk, renal function, risk of hypoglycemia, and weight.1
Hypoglycemia is also associated with reduced cognitive function. Individuals with poor cognitive function have more severe hypoglycemia. A long-term study of older patients with type 2 diabetes demonstrated that individuals with one or more recorded episodes of severe hypoglycemia had a stepwise increase in their risk of dementia. Similarly, as cognitive function decreases, the risk of severe hypoglycemia increases. Therefore, it is important to tailor glycemic therapy to help prevent hypoglycemia in individuals with cognitive dysfunction.1
Individuals who are anxious or concerned about diabetes complications or treatment should be screened for anxiety, which may interfere with important facets of self-management. Patients who are insufficiently aware of or who fear hypoglycemia will benefit from education and training to help them become more aware of the importance of self-management.1
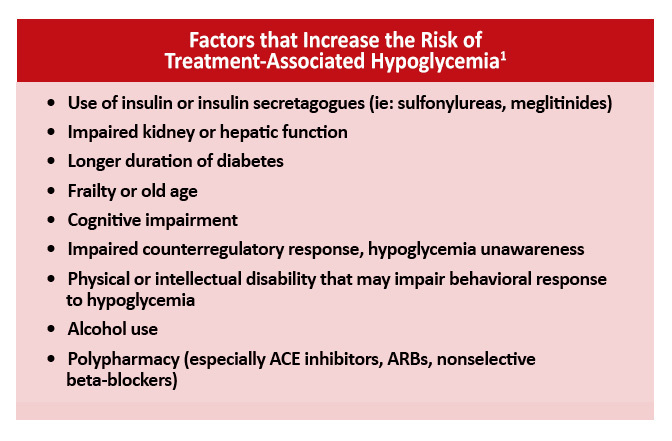
Risk Factors for Hypoglycemia
It is important when selecting therapy options that physicians assess a patient’s risk of hypoglycemia.
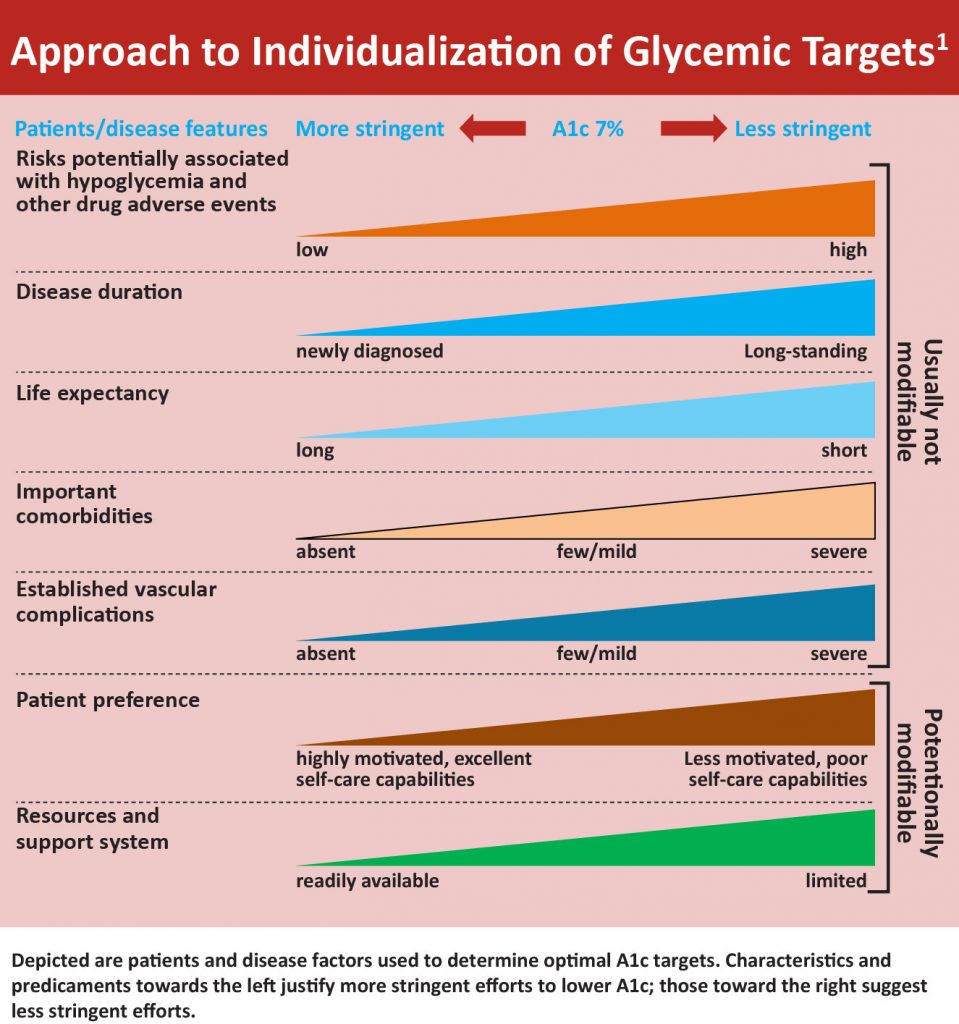
HbA1c Goals
New guidelines emphasize the need to tailor treatment to each individual. The 2019 Standards of Medical Care in Diabetes notes that less stringent A1c goals (such as <8% [64 mmol/mol]) may be appropriate for patients who have a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, significant comorbid conditions, or long-standing diabetes that has been difficult to control despite self-management education, appropriate glucose monitoring, and appropriate doses of multiple agents, including insulin.1 A more stringent A1c goal (such as <6.5% [48 mmol/mol]) may be appropriate for patients who are at low risk for hypoglycemia, such as patients with short duration of diabetes, type 2 diabetes managed with lifestyle or metformin alone, long life expectancy, or no significant cardiovascular disease. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens and the setting of higher glycemic goals.1
The results of key trials—ACCORD, ADVANCE, and VADT—reveal that elderly patients may not experience macrovascular benefits from aggressive glycemic control. Intensive therapy was associated with increased risk of severe hypoglycemia and potential increases in mortality.1
The landscape for effective diabetes management has changed greatly over the past decade. To provide optimum care, clinicians need in-depth knowledge of currently available agents, their mechanism and onset of action, and most common adverse effects, especially the frequency of hypoglycemia. They must be able to adjust medication and class of medication appropriately as needed.
A stepwise approach to the management of hypoglycemia is shown in the Figure.
Glucose Lowering Drugs
Oral agents, such as sulfonylureas, present the greatest risk of hypoglycemia. A switch to newer classes or new generations of agents should be considered for patients who are at elevated risk for hypoglycemia or who have experienced an event.
The risk of hypoglycemia typically increases with the duration of insulin use. Five years after the initiation of insulin therapy, the rate of severe hypoglycemia has been reported to reach 35 to 70 episodes per 100 patient-years.2 Counterregulatory responses to hypoglycemia decline with frequent and repetitive episodes; repeated episodes can impair defenses against subsequent episodes and increase the risk of both recurrences and mortality.2 Older adults with known cardiovascular disease are at particular risk.1
Newer insulin products differ in their pharmacokinetic/pharmacodynamic profiles. Basal insulin features a more stable pharmacodynamic profile and enables patients to safely target normal-range fasting blood glucose by providing a consistent glucose-lowering effect to reduce the occurrence of hypoglycemia.3
One class of agents shown to have a positive effect on glycemic control and to reduce the risk of hypoglycemia and cardiovascular effects is the glucagon-like peptide-1 (GLP-1) receptor agonist. These agents, which act on the incretin axis, have additional benefits for weight loss, systolic blood pressure, and renal function. Patients who wish to lose weight or avoid weight gain may benefit from this option. The glucose-dependent mechanism of action characteristic of this class of medications has the advantage of exhibiting a lower risk and incidence of hypoglycemia.5 Nonglycemic effects positively influence gastric emptying and satiety. The most commonly reported adverse events include dose-related nausea, diarrhea, and vomiting. These effects typically subside over time.4
Sodium-glucose cotransporter 2 (SGLT-2) inhibitors feature an insulin-independent mechanism of action and provide an intermediate lowering of A1c. Some agents have been shown to be associated with positive cardiovascular outcomes.6–8 Compared with active comparators (eg, metformin, sulfonylureas, and/or sitagliptin), some SGLT-2 inhibitors show similar or greater reductions in A1c and are associated with significant reductions in body weight and systolic blood pressure,7 as well as positive renal outcomes.9,10
Hyperglycemia Unawareness
Hyperglycemia unawareness is a syndrome characterized by deficient counterregulatory hormone release and diminished autonomic response caused by episodes of hypoglycemia. This dysregulation places individuals at risk for additional hypoglycemic events for several days or weeks. Hypoglycemia unawareness is characterized by a failure of epinephrine and glucagon release, preventing mobilization of endogenous glucose stores from the liver.11 This cycle can be stopped if several weeks without hypoglycemia can be achieved. Hence, to prevent future episodes of hypoglycemia, patients with one or more episodes of clinically significant hypoglycemia may benefit from at least short-term relaxation of glycemic targets.1
References
- American Diabetes Association. Standards of Medical Care in Diabetes – 2019. Diabetes Care. 2019;42(Suppl 1):S90-S102.
- Evert AB. Treatment of mild hypoglycemia.Diabetes Spectr. 2014;27:58-62.
- Marso SP, McGuire DK, Zinman B, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377:723-732.
- Blonde L. Achieving antihyperglycemic treatment goals with incretin-related therapies. Am J Manag Care.2012;18(10 suppl):S219-S227.
- Lindamood CA, Taylor JR. Emerging new therapies for the treatment of type 2 diabetes mellitus: glucagon-like peptide-1 receptor agonists. Clin Ther.2015;37:483-493.
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117-2128.
- Liakos A, Karagiannis T, Athanasiadou E, et al. Efficacy and safety of empagliflozin for type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2014;16:984-993.
- Zhang XL, Zhu QQ, Chen YH, et al. Cardiovascular safety, long‐term noncardiovascular safety, and efficacy of sodium-glucose cotransporter 2 inhibitors in patients with type 2 diabetes mellitus: a systemic review and meta‐analysis with trial sequential analysis.J Am Heart Assoc. 2018;7:e007165.
- Staels B. Cardiovascular protection by sodium glucose cotransporter 2 inhibitors: potential mechanisms. Am J Cardiol. 2017;120(1 suppl) :S28-S36.
- Wanner C. EMPA-REG outcome: the nephrologist’s point of view.Am J Cardiol.2017;120(suppl 1):S59-S67.
- Samson WK, Stein LM, Elrick M, et al. Hypoglycemia unawareness prevention: targeting glucagon production. Physiol Behav. 2016;162:147-150.

