Frequently Asked Questions
How are type 1 and type 2 diabetes different?
Insulin is a hormone made in the body that works by moving glucose (a specific type of sugar) from the bloodstream into the cells of the body. The cells of the body need glucose for energy to perform normal functions. Patients with type 1 diabetes do not produce insulin, posing a problem when it comes to delivering much needed energy to the body’s cells. This is the reason why insulin therapy is used for treating type 1 diabetes.1
Patients with type 2 diabetes have the ability to produce insulin, but their bodies cannot use insulin properly, limiting the amount of fuel (glucose) the cells receive while increasing the amount of glucose in the blood. When this happens, blood glucose readings will be higher than normal, sometimes resulting in the need for drug therapy in addition to lifestyle modifications. Unlike patients with type 1 diabetes, those with type 2 diabetes typically do not start drug therapy using insulin. But, as the condition gets worse, insulin therapy may be needed to control blood glucose levels.2
Type 1 diabetes is usually diagnosed in children and young adults and makes up about 5% of people with diabetes.1
References:
- American Diabetes Association. Type 1 diabetes. Available at http://www.diabetes.org/diabetes-basics/type-1/ Accessed: May 2019
- American Diabetes Association. Type 2 diabetes. Available at http://www.diabetes.org/diabetes-basics/type-2/ Accessed: May 2019
Are type 1 and type 2 diabetes treated the same way?
Type 1 diabetes treatment begins with insulin therapy. Treatment for patients with type 2 diabetes depends on a range of factors and always includes lifestyle changes, such as increasing exercise and healthy eating.1
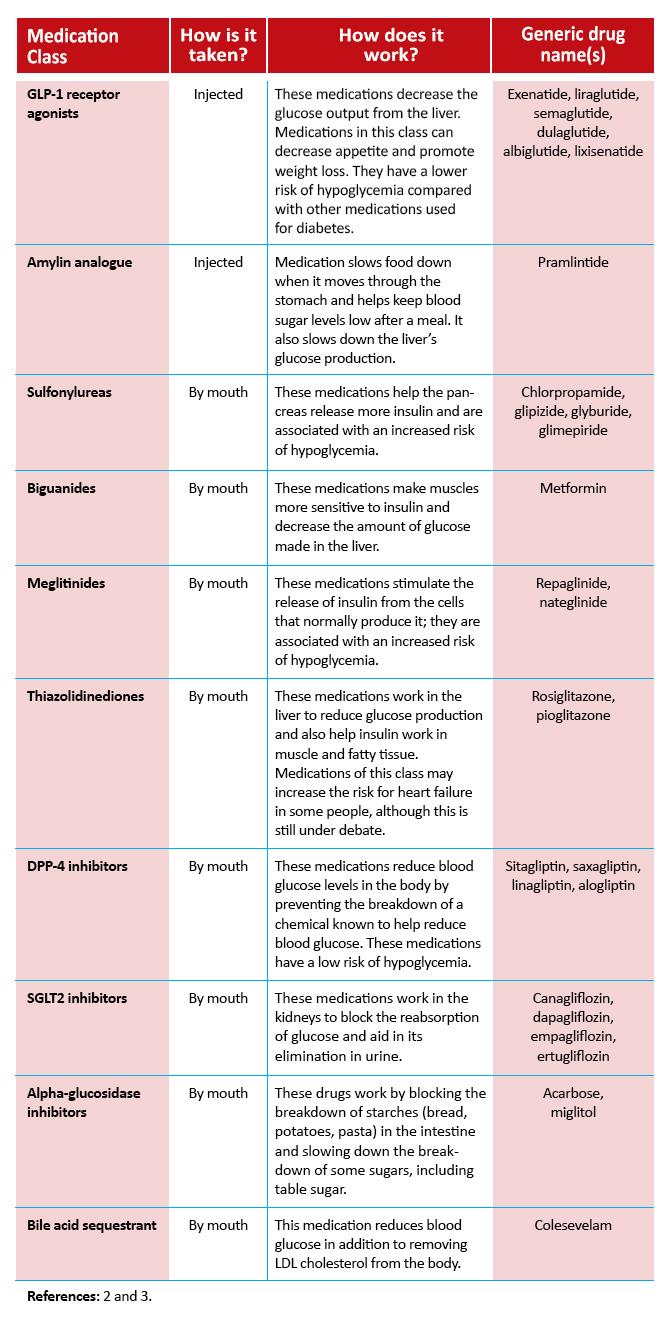
Other drugs besides insulin that are used to treat diabetes can be found in the table below. Decisions on which medication is best for each patient depends on a variety of factors that must be explored by individual patients and their healthcare team.
References:
- American Diabetes Association. Medication. Available at http://www.diabetes.org/living-with-diabetes/treatment-and-care/medication/ Accessed in May 2018.
- American Diabetes Association. Other injectable medications. Available at org/living-with-diabetes/treatment-and-care/medication/insulin/other-injectable-medications.html. Accessed in May 2018.
- American Diabetes association. What are my options? Available at diabetes.org/living-with-diabetes/treatment-and-care/medication/oral-medications/what-are-my-options.html. Accessed in May 2018.
Do all medications used for diabetes cause hypoglycemia?
Some medications used to treat diabetes may increase the risk of hypoglycemia. Monitoring blood glucose closely and knowing how blood glucose monitors work are crucial to correctly evaluating blood sugar levels.1
Although insulin has the highest risk of hypoglycemia, other medications, such as sulfonylureas, may be associated with an increased risk of hypoglycemia. Make sure to discuss the risks for hypoglycemia with your healthcare team in order to come up with the most effective treatment plan for you.2 Other factors that can influence hypoglycemia risk include missed or irregular meals, incorrect use of diabetes medication (dose or timing), changes in physical activity, and alcohol.2
- If your blood sugar is not controlled. Available at https://www.cornerstones4care.com/medicine/what-to-do/uncontrolled-blood-sugar.html. Accessed in May 2018.
- Lingvay I. Hypoglycemia in type 2 diabetes—consequences and risk assessment. US Endocrinol. 2011;7:95-102.
Are there ways to stop hypoglycemia?
Preventing low blood sugar is just one of the many important factors that come into play when treating and managing hypoglycemia. Talk with your healthcare team to discuss treatment options if you are experiencing hypoglycemia that you think may be caused by your medication.1
Other ways to prevent hypoglycemia include1:
- National Institute of Diabetes and Digestive and Kidney Diseases. Low blood glucose (hypoglycemia). Available at www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/low-blood-glucose-hypoglycemia. Accessed in May 2018.
WHAT DO MY A1c RESULTS MEAN?
Your A1c is an estimate of your average blood glucose level over the past 2 or 3 months. When you test your blood glucose with a glucose meter, you are measuring your blood sugar level at that one moment. This number varies throughout the day and it is important in determining if you are experiencing an episode of hypoglycemia or hyperglycemia. For example, your blood glucose may rise after you eat and fall after you exercise. Your A1c changes gradually and gives you a better idea of whether your diabetes treatment plan is working to control your blood glucose level over time.
Your A1c will be tested at least twice a year. The A1c test measures the amount of sugar on hemoglobin molecules in your red blood cells. Hemoglobin is a molecule in your red blood cells that carries oxygen to your cells. Glucose in your body enters your red blood cells and attaches to hemoglobin. The more glucose in your bloodstream, the more sugar attached to the hemoglobin.
An A1c level below 5.7% is considered normal. Patients with A1c levels between 5.7% and 6.4% have prediabetes. Diabetes is defined as A1c levels of 6.5% or above. Your A1c may be used by your healthcare team to set your treatment goals, modify your therapy, and monitor your diabetes management. Most people with diabetes should try to achieve an A1c target under 7%. This target has been shown to reduce the risk of diabetic complications in several studies.
However, the A1c goal should be personalized for each patient. An A1c between 7% and 8%, or even higher, may be appropriate for patients at risk of severe hypoglycemia or for patients who are unable to sense the symptoms of hypoglycemia (also known as hypoglycemia unawareness). Your A1c target may change over time depending on personal factors.
Resources
- National Institute of Diabetes and Digestive and Kidney Diseases. The A1c Test & Diabetes. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis/A1c-test#whatis
- American Diabetes Association. A1c and eAG. http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/a1c/
HOW DO I TREAT EPISODES OF HYPOGLYCEMIA?
In order to treat hypoglycemia, you must quickly raise your blood sugar levels. The best way to do that is to use the “15-15 Rule.”
The “15-15 Rule” is simple. Consume 15 grams of carbohydrate to raise your blood glucose and check your level after 15 minutes. If your blood glucose level is still below 70 mg/dL, take another 15 grams of carbohydrate. Repeat these steps until your blood glucose is at least 70 mg/dL. Once your blood glucose is back to normal, eat a meal or snack to make sure your glucose levels don’t drop again. Do not eat too much or your glucose levels may shoot too high!
Some examples of quick sources of carbohydrate include:
- Glucose tablets (can be purchased at a local pharmacy)
- Gel glucose (can be purchased at a local pharmacy)
- 4 ounces (1/2 cup) of fruit juice or regular soda (not diet)
- 1 tablespoon of sugar, honey, or corn syrup
- Hard candies, jellybeans, or gumdrops (read the food label to see how many to consume)
Avoid using complex carbohydrates, such as pasta, or foods that contain fat along with sugar, such as chocolate. These foods can slow the absorption of glucose and should not be used in an emergency.
The “15-15 Rule” applies to adults. Young children usually need less than 15 grams of carbohydrate to increase their blood glucose level. Discuss the amount of sugar your child needs to correct hypoglycemia with your doctor. Infants may need only 6 grams of carbohydrate, toddlers may need 8 grams, and small children may need 10 grams.
Be sure to tell your doctor if you experience an episode of low blood sugar. They may suggest ways to avoid hypoglycemia in the future.
Resources
- American Diabetes Association (ADA). Hypoglycemia (Low Blood Glucose). http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hypoglycemia-low-blood.html?loc=lwd-slabnav
HOW DO I TREAT SEVERE HYPOGLYCEMIA?
Severe hypoglycemia is a dangerous event caused by very low blood glucose levels. Hypoglycemia is considered severe if you require assistance from another person to treat it.
Treatment for severe hypoglycemia consists of an injection of glucagon. Glucagon is a hormone produced by the pancreas that stimulates your liver to release stored glucose into your bloodstream. Glucagon is available by prescription. Speak to your doctor about whether you should get a glucagon kit and how and when to use it. It is important that people who are frequently around you know how to give you a glucagon injection if needed. This includes family, friends, coworkers, teachers, and others.
Glucagon should be injected into the buttock, arm or thigh, following the instructions in the kit. The person will regain consciousness within 5-15 minutes, but may experience nausea and vomiting. Be sure to tell your doctor if you experience severe hypoglycemia as this is a life-threatening complication of diabetes.
Do not try to give someone experiencing severe hypoglycemia food or juice. They may choke. Do not give them an insulin injection as that will lower their blood sugar even more.
Do not hesitate to call 911.
Resources
- American Diabetes Association (ADA). Hypoglycemia (Low Blood Glucose). http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hypoglycemia-low-blood.html?loc=lwd-slabnav
WHAT IS HYPOGLYCEMIA UNAWARENESS?
Most people with diabetes experience symptoms of hypoglycemia if their blood glucose levels fall below 70 mg/dL. These symptoms may include feeling shaky or lightheaded, headaches, anxiety, sweating, chills, and others. However, some people may not feel any symptoms even though their blood glucose levels are low. This is called hypoglycemia unawareness.
Hypoglycemia unawareness puts a person at increased risk of severe hypoglycemia. If a person is unable to feel symptoms of hypoglycemia, they may not know to treat it. People with hypoglycemia unawareness need to take extra precautions to check their blood glucose frequently, particularly before dangerous activities such as driving.
Hypoglycemia unawareness is more common in people who:
- Frequently have low blood glucose episodes
- Have had diabetes for a long time
- Tightly control their diabetes
If you think you may have hypoglycemia unawareness, speak with your healthcare team. They may adjust your blood glucose targets to minimize your risk of hypoglycemia in the future. They may also recommend the use of a continuous glucose monitor that sounds an alarm when blood glucose levels are low.
It is possible to regain your ability to sense hypoglycemia. Your body may re-learn how to react to low blood glucose levels by avoiding any, even mild, episodes of hypoglycemia for several weeks. Your healthcare team may recommend higher blood glucose targets to prevent the risk of hypoglycemia during this period.
Resources
- American Diabetes Association (ADA). Hypoglycemia (Low Blood Glucose). http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hypoglycemia-low-blood.html?loc=lwd-slabnav
WHAT QUESTIONS SHOULD I ASK MY DOCTOR ABOUT HYPOGLYCEMIA?
Talking often with your healthcare team and asking questions are important for making informed decisions about your health. There is no one-size-fits-all approach to treating diabetes. It is vital that you receive personalized information about your blood glucose goals and health. Many people feel anxious about questioning their doctor or worried that they may not understand medical terms. The following strategies may help you talk to your doctor and get the information you need:
- Take someone with you to doctor visits who can take notes, listen, and ask questions.
- Ask as many questions as you need to. Write down your questions and bring them with you to appointments.
- Remember that all of your questions are important. There is no such thing as a silly question when it comes to understanding your health.
- Ask the doctor to explain any medical terms you don’t understand and write down any terms you don’t know.
- Repeat back the information the doctor gives you in your own words to make sure you understand it.
Minimizing the risk of hypoglycemia is an important goal in the management of diabetes. The following is a list of questions about hypoglycemia that you may want to ask your doctor. Remember to write down any additional questions you have about your own health and bring them with you to your appointment.
- Are my signs and symptoms caused by hypoglycemia?
- What do you think is triggering my hypoglycemia?
- Do I need to adjust my medications or treatment plan?
- Do I need to make changes to my diet?
- Do I need to make changes to my exercise routine?
- What are some possible complications of hypoglycemia?
- How can I better monitor my blood glucose levels?

